-
 Customers success stories
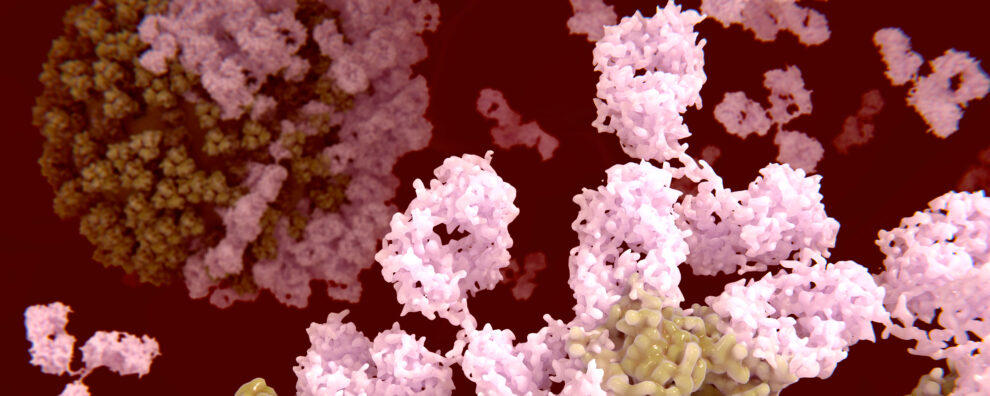
Customers success storiesThe Path of Creating an Innovative IL-17A Antibody for Autoimmune Disorders
At ProteoGenix, we are devoted to promoting innovative research and offering superior solutions that assist our clients in reaching their scientific objectives. Our client at the University of Naples and…
-
CAR-T cell therapy
From the first to the fifth generation of CAR-T cells
Read more -
CAR-T cell therapy
The structure of CAR-T cells
Read more -
Antibody-drug conjugates
Robust methods for the detailed analysis of drug-to-antibody ratio (DAR) and drug load distribution
Read more -
Antibody-drug conjugates
ADC payloads
Read more -
Antibody-drug conjugates
How to choose the best linker for an ADC? Cleavable vs. non-cleavable
Read more
-
Customers success stories
The Path of Creating an Innovative IL-17A Antibody for Autoimmune Disorders
Read more -
Antibody production
Polyclonal vs. Monoclonal antibodies: How to choose the best option for your project?
Read more -
Antibody production
How to choose the best antibody generation technique for your project?
Read more -
Antibody production
The best CHO expression system kits on the market
Read more -
Antibody production
A guide on how to easily transition to a new antibody expression system kit
Read more
-
Antibody production
“The COVID-19 pandemic is helping us bridge the divide between virologists and immunologists”
Read more -
Antibody production
Reinventing IgY biotherapeutics
Read more -
Antibody production
How the environment shapes immune system development during pregnancy
Read more -
Antibody production
“Cell-based phage display is helping us isolate more biologically relevant antibodies”
Read more -
Antibody production
“Researchers are not leveraging the speed and resolution of flow cytometry for clinical evaluation”
Read more