 Antibody production
Antibody production
“The COVID-19 pandemic is helping us bridge the divide between virologists and immunologists”
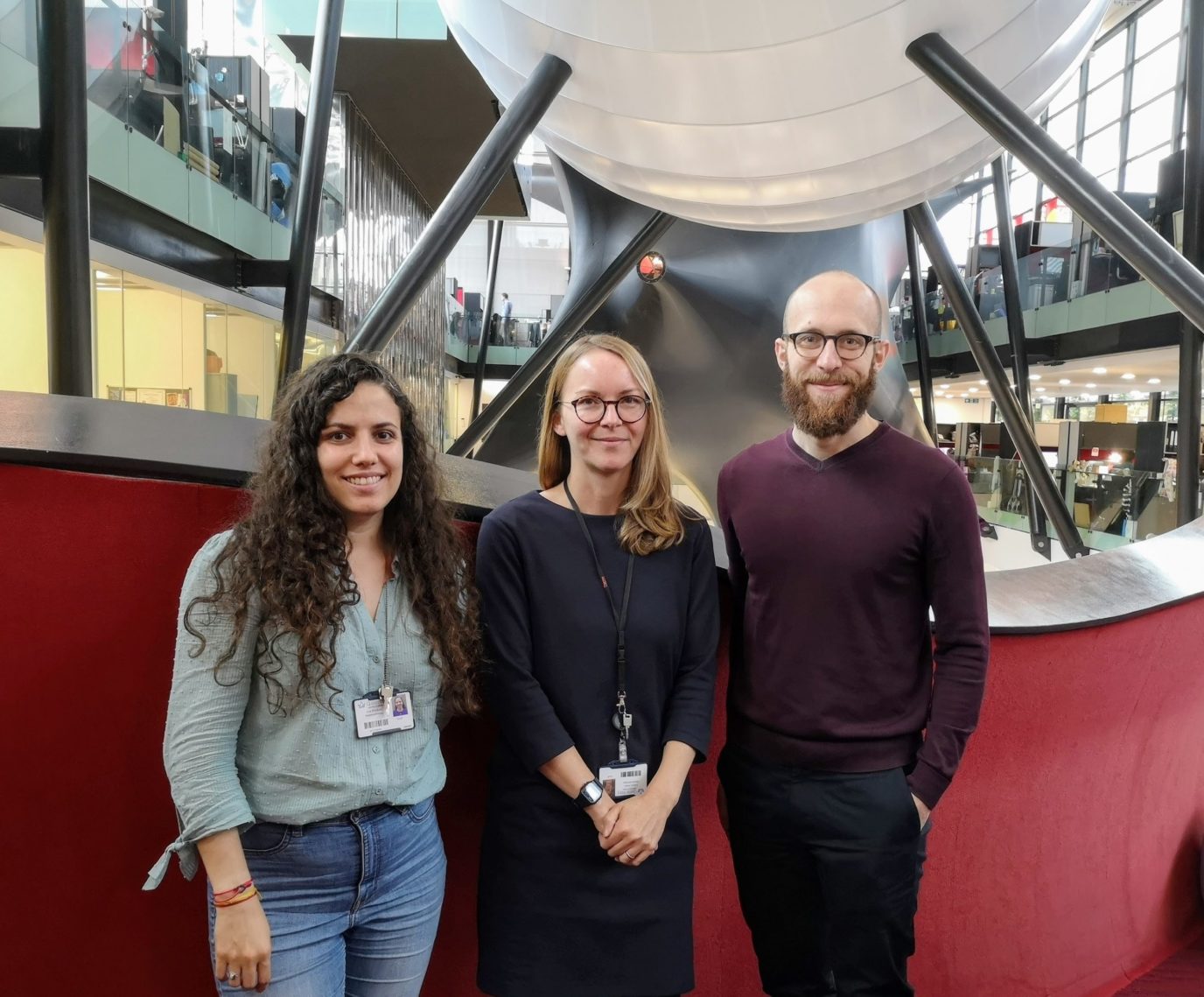
An autoimmune disorder and natural curiosity led Dr. Louisa James to a fascinating career in immunology. Dr. James is currently a group leader and lecturer at the Blizard Institute from the Queen Mary University of London (QMUL, UK) where she has spent a great part of her career pursuing unanswered questions about B cell biology. We have spoken with Dr. James about her fascinating discoveries in B cell regulation and explored topics such as the COVID-19 pandemic, allergen immunotherapy, and how her discoveries might impact the future of immunotherapy and vaccination in the decades to come.
- Starting with your academic journey, when and how did you become interested in the study of allergy and autoimmunity?
- You have devoted a great part of your career to the study of B cell memory regulation. On a personal and professional level, what fascinates you the most about this topic?
- You have recently published a highly impactful study on Science Immunology regarding B cell biology [1]. What prompted this study in the first place? What questions did you attempt to answer?
- Which of these new research avenues do you want to continue pursuing?
- As you said before, you encountered a lot of technical challenges throughout this study. Can you tell us more about them?
- What about the tools you referred to earlier to analyze antigen-specificity?
- In some of your earlier works, you have also explored topics such as allergen injection immunotherapy [2]. What were your most important findings regarding this therapeutic approach?
- Is allergen immunotherapy a widespread clinical practice for reducing and managing allergies? And if not, what is hindering its widespread application?
- You have recently participated in a large study assessing the immune repertoire of COVID-19 patients [3]. What was your role in this study and how does it relate to your previous research on allergy and autoimmunity?
- Can you summarize the most important findings of this study? How do you think it will impact the ongoing and future pandemics?
- After this experience, what do you think virologists can learn from immunologists and vice-versa?
- Throughout your impressive career, what do you consider to be your greatest or more interesting findings?
- What other projects are happening in your lab at the moment?
- What are your goals, research-wise, for the next 10 years?

Starting with your academic journey, when and how did you become interested in the study of allergy and autoimmunity?
When I was 11, I was diagnosed and hospitalized with autoimmune liver disease. I was quite lucky because the disease is stable and has relatively unaffected my life. Yet that disease led me to Professor Giorgina Mieli-Vergani, the hepatologist and immunologist who handled my case. She was also the Head of Paediatric Liver Research at King’s College Hospital and I kept asking her questions. One day, she took me to her lab where I spent the afternoon with her postdoc, who is now a Professor at Yale called Li Wen. I’ve never been to a lab before and I was just fascinated.
From that age onward, I think all I wanted to do was work in a lab. So, when the time came to apply to University, I knew I wanted to study immunology. It was a fascinating topic that I ended up pursuing due to the encouragement of my exceptional science teachers.
It was during my undergraduate degree that I became interested in allergy simply because we had great teachers and guest speakers who gave fascinating lectures on the topic. When I finished my undergrad studies, I knew I wanted to pursue this topic further and thus applied to a Ph.D. in allergy. Soon after, I started my career as a researcher in allergy by studying a type of treatment called allergen immunotherapy. Then, I brought that know-how to my postdoc where we investigated the use of peptide immunotherapy for diabetes. I studied diabetes and the use of antigen-specific treatments to change the immune response to the disease for a few years. But I eventually missed studying allergy, so I did my second postdoc on that topic and stayed in the field ever since.
You have devoted a great part of your career to the study of B cell memory regulation. On a personal and professional level, what fascinates you the most about this topic?
During my Ph.D., the hot topic was T cell regulation, so I did a lot of work on T cell biology and antibodies at the time. When I went back to allergy for my second postdoc, I was lucky to join the lab of Professor Hannah Gould who is an expert on IgE and that was where I dove deeply into B cell biology for the first time.
Up until that point, most of my work had been at a cellular level using tools like flow cytometry. My work at Gould’s lab was my first experience in molecular immunology. There I found just how fascinating B cells could be. The more you learn about them, the more interesting they become. These cells are constantly learning and adapting. They can become long-lived and the molecular processes they have to undergo to achieve that are fascinating. But what eventually persuaded me to continue studying B cells at my lab was the number of unanswered questions regarding their biology.
Of course, we know a lot about the mechanics behind the biology of these cells like DNA rearrangements, class switch recombination, and somatic hypermutation. But a lot of the decision-making process is still unclear. And those open questions were the ones that drove me to keep studying B cells.
You have recently published a highly impactful study on Science Immunology regarding B cell biology [1]. What prompted this study in the first place? What questions did you attempt to answer?
The fundamental question we had at the beginning of this study was: if you take memory B cells expressing different antibody subclasses, can you observe differences in their phenotypes? In other words, do B cells expressing IgG2 have different measurable properties from cells expressing IgG4?
We knew these questions could only be answered by single-cell techniques and that was a great motivation for this study. For this purpose, we sampled tonsils from different individuals because we knew they were a good source of B cells. As a consequence, we ended up generating a massive dataset that is still helping us understand a lot of the central processes of B cell biology.
These answers were slightly different from what we had anticipated at the beginning of the study. Instead of detecting phenotypical differences, we ended up describing the germinal center response of B cells in a lot more depth than what had been achieved before. To some extent, I have not answered that original question, but the results we gathered were so fascinating, they opened further research avenues.
Which of these new research avenues do you want to continue pursuing?
This study showed us we need to reassess what we know about different B cell states. What makes a B cell express certain genes and not others is a question we still can’t answer. The context where these B cells have been activated could help explain the differences. But what remains to be answered is whether this is related to antigen specificity. Our goal at the moment is to try to understand that connection.
In this study, we didn’t have the opportunity to look at B cell specificity due to technical limitations. This is something we would like to pursue now that the tools to ask these questions are becoming available. These new tools will allow us to combine techniques to interrogate specificity with techniques we have been using until now to study gene expression.
Other surprising results of this study were the new insights into class switching mechanisms. We knew from previous studies, particularly from Carola Vinuesa’s lab, that class switching can occur before the germinal center response is initiated. Surprisingly, in this study, we identified this subpopulation of cells undergoing that process. What remains to be answered is: what’s driving that class switching event? Answering that question will potentially change the way we perceive the germinal center response. Plus, it might also help us understand how to manipulate these cells for the design of more effective vaccination strategies.
As you said before, you encountered a lot of technical challenges throughout this study. Can you tell us more about them?
On a personal level, my background was primarily cellular biology and immunology. Before this study, I’ve had experience with antibody repertoire sequencing but the techniques we used for this study – single-cell RNA sequencing – were on a completely different level in terms of data analysis. The mathematical tools to analyze the two types of data are vastly different.
I was very lucky because back when I started my lab in 2016, I managed to recruit an excellent postdoc – Hamish King – who has been working with me ever since he finished his Ph.D. in a genomics lab. Having worked with genomics, Hamish had a lot of experience doing bioinformatic analysis but he also combined that with wet lab work. He takes the credit for all the computational part of this study due to this background and the time he spent in Sarah Teichman’s lab to learn how to implement the packages they had developed for single-cell data analysis. Teichman and her team had developed a lot of tools for the Human Cell Atlas project, and Hamish was able to develop them further for our specific data.
That was the biggest challenge we faced during this study. But I was happy to have members at my lab who were able to handle this data and do something impressive in terms of analysis.
What about the tools you referred to earlier to analyze antigen-specificity?
Conventionally, antigen-specificity can be interrogated by labeling antigens with fluorophores and then analyzing antigen-B cell complexes by flow cytometry.
In the past year, a group led by Ivelin Georgiev came up with a different strategy. Instead of attaching a fluorophore to an antigen, they attached a barcode in form of a DNA sequence, that can be integrated into a single-cell sequencing pipeline. In this case, when the cell is captured, if it is bound to an antigen that barcode becomes incorporated in the sequence and can be identified by computational techniques.
This raises the scope of possibilities because with flow cytometry we were limited to 30 colors/antigens, but the use of barcodes has lifted that limitation. Some of the questions we are now trying to answer are suited for this high-throughput approach.
In some of your earlier works, you have also explored topics such as allergen injection immunotherapy [2]. What were your most important findings regarding this therapeutic approach?
Allergen immunotherapy has been around for over 100 years. When it was first tested, IgE and its role in allergy hadn’t been discovered. But vaccines were fast becoming one of the most important tools in public health. At the time, doctors devised a vaccine-based strategy to treat hay fever, thought to be caused by a toxin from grass pollen. The premise behind injecting small amounts of grass pollen was that it would vaccinate people against that toxin.
We now know hay fever is a reaction to grass pollen itself and not a response to a toxin. But that treatment worked. It reduced symptoms and, for this reason, it continued being used for the next 100 years. But we didn’t understand why it worked nor the principles of the allergic response.
I started working on allergen immunotherapy during my Ph.D. by focusing on the T cell regulatory response. By then, we knew IgE was the main mediator of allergies, but we were also interested in IgG4 due to its strong effect on the regulation of allergy responses.
IgG4 is a fascinating subclass of IgG antibodies. It doesn’t induce any inflammatory response nor does it bind well to Fc-receptors or complement. But IgG4 antibodies have this amazing trick called Fab-arm recombination where the two arms of an antibody separate and recombine with other IgG4, creating natural bispecific antibodies.
What does it mean in terms of function? It means these antibodies cannot crosslink with identical antigens, also known as functional monovalency. This response only happens after chronic allergen exposure or when patients receive allergen immunotherapy.
For a long time, this response was considered important because clinical studies had shown that IgG4 levels would drop as soon as patients stopped receiving immunotherapy despite them remaining symptom-free. When total IgG4 was measured, these antibodies appeared to correlate poorly with the immune response. So, most researchers assumed IgG4 was simply a marker of exposure but unimportant for the modulation of the allergic response.
During my Ph.D. and subsequent research, I focused on showing the importance of IgG4 antibodies. What we found was that the absolute concentration of IgG4 was less important than the quality of IgG4-mediated responses. This means that even if the concentration of these antibodies falls after exposure, what you retain is of sufficient affinity to block the key epitopes of an allergen, thus preventing IgE from inducing the allergy response. Now, the importance of IgG4 in allergy regulation is widely recognized. And there is even an IgG4 antibody in Phase III clinical trials that binds cat dander – an allergen from cats. This antibody, once approved, will serve as a passive therapy in patients with cat allergy and those advances are truly exciting.
Is allergen immunotherapy a widespread clinical practice for reducing and managing allergies? And if not, what is hindering its widespread application?
The situation differs from country to country. In the UK, for example, allergen immunotherapy is limited to patients who have severe allergies, are not at high risk of anaphylaxis, and are unresponsive to conventional treatments like antihistamines. Why these restrictions? In some patients, allergen immunotherapy can trigger adverse allergic responses and lead to anaphylaxis. Those responses are manageable and can easily be reverted. However, because of this risk, patients who receive immunotherapy have to receive these injections in hospital settings and stay for observation up to 1 hour after injection to ensure no adverse reactions take place.
Despite the downsides, allergen immunotherapy works well. More importantly, as long as patients have received at least 2 years’ worth of treatment, the protective effects persist for a long time.
These treatments are so successful because they modify the immune response to an allergen. But to make these treatments more accessible to the general population, safer forms of immunotherapy must be created. In past decades, an alternative form of immunotherapy has been licensed. It is called sublingual immunotherapy (SLIT) and it consists of a daily tablet patients can take at home. This makes it much safer than conventional injection immunotherapies. Besides SLIT, other forms of treatment are being tested for severe food allergies. Once these treatments enter the market, immunotherapy is likely to become more widespread.
You have recently participated in a large study assessing the immune repertoire of COVID-19 patients [3]. What was your role in this study and how does it relate to your previous research on allergy and autoimmunity?
The Queen Mary University of London is part of a medical school and it is closely associated with hospital trusts. One of the closest trusts to where I work is the Royal London Hospital, one of the biggest hospitals in the country.
When the COVID-19 pandemic started, the Royal London Hospital quickly became a central point for COVID-19 patients. At that time, I already worked closely with a few of my colleagues in respiratory health, asthma physicians at the hospital who operated on the frontline of the COVID-19 response. During that time, Alchemab Therapeutics Ltd. approached my colleagues and asked if they could collect samples from COVID-19 patients to carry out antibody discovery studies using repertoire sequencing. Because of the lockdown, I was working from home but since the study involved patients at the Hospital trust, I was invited to participate in data analysis and interpretation. It was a fascinating opportunity that embodies the impressive level of collaboration we have witnessed during the past year in terms of COVID-19 efforts.
Can you summarize the most important findings of this study? How do you think it will impact the ongoing and future pandemics?
In this study, we were looking for convergent signatures in antibody responses. The most amazing property of antibody repertoires is their immense diversity across populations. But it has been known for a while that some infectious diseases can cause a convergence of particular rearrangements of antibodies even among patients with vastly different repertoires.
Knowing this helps because one of the disadvantages of doing high-throughput sequencing is the inability to interrogate antibody specificity, but you can instead detect overlaps between different individuals. These overlaps are the sign of convergent signatures and often lead to the identification of antibodies with clinical relevance.
What we showed in this study was evidence of convergence in immune responses to the COVID-19 disease. These findings will be useful to understand and respond quickly to future diseases caused by coronaviruses and even future pandemics. In practical terms, therapeutic antibody discovery by convergent signature analysis has proven to be another valuable arm on our discovery toolkit. These tools are available and ready to be harnessed quickly in future infectious disease outbreaks.
After this experience, what do you think virologists can learn from immunologists and vice-versa?
There has sometimes been a divide between pure virologists and pure immunologists. But in terms of the COVID-19 response, virologists and immunologists have been quite aligned when advising the government regarding lockdown measures and, more recently, in terms of vaccination policies. To some extent, the COVID-19 pandemic is helping us bridge those differences.
From a practical point of view, technical progress has also contributed to reducing that divide. The reason is that researchers can now take a much more unbiased approach to data analysis. It is now possible to ask very specific and unbiased questions in a disease context, whether it’s to unravel a new pathway or discover a new mechanism. These advanced techniques have made research much more open to discovery science. A type of science that has been traditionally very hard to attract funding for.
As a consequence, our understanding of the underlying mechanisms of infection and autoimmunity increased exponentially. For example, it is now very clear there is a strong relationship between the sort of immune responses activated in the context of infection and autoimmunity. The discovery of these relationships will shape the future of both fields of study. As a result, soon we will witness a huge amount of progress, not only in the mechanistic aspects but also in how to apply that knowledge to design better therapies.
Throughout your impressive career, what do you consider to be your greatest or more interesting findings?
That’s a very difficult question! In terms of what I’m most proud of, I would choose our most recent paper in Science Immunology [1]. A vast amount of interesting data came out of this study out of pure curiosity and in an attempt to answer many open questions regarding B cell biology. We weren’t able to answer that fundamental question. But we came out of this study with a rich resource of data that is still taking us to new questions.
One of the most interesting outcomes of this study resulted from publishing the data on bioRxiv. Since then, a lot of researchers have reached out to us asking to use that data for various other projects. Knowing this data remains useful in different contexts is something my team and I can be proud of.
What other projects are happening in your lab at the moment?
In terms of lab work, projects have been progressing slowly for the past year due to the COVID-19 pandemic. Much of our work has become digital. But one interesting outcome of this “migration” happened back in May 2020 when we first published our study on bioRxiv. Because we shared our data early on, a group at Stanford University (US) contacted us. They had done some work on B cells including fascinating studies using genome-wide association data and were interested in collaborating. So, during the lockdown, Hamish had the opportunity to work closely with them and the result is our latest pre-print on bioRxiv [4] that is also in the process of peer-review.
Taking advantage of the lockdown, I’m also using this time to set up future work on high-throughput antibody specificity at my lab. Plus, I have many ongoing collaborations with other labs where we’re investigating antibody cloning, carrying out antibody repertoire analysis in the context of multiple human diseases, and pursuing further studies on food allergy and autoimmunity.
What are your goals, research-wise, for the next 10 years?
My focus at the moment is getting this new project on specificity up and running. In addition to that, I’m interested in resuming my studies in respiratory diseases, particularly the ones that affect the upper airway.
The main goal for the next 5-10 years is trying to understand where B cell dysregulation happens and how these mechanisms arise in chronic respiratory diseases and how they are related to antigen-specificity.
The initial motivation for our study published in Science Immunology was to have a better grasp of B cell biology. That study became a stepping stone in our goal to understand B cell responses in disease contexts. For example, we know patients with respiratory diseases are more susceptible to infection, but we don’t know whether this susceptibility correlates or not with dysregulation of the antibody response. So, there’s a lot of work ahead of us on that front.
Another goal I have for the next years has to do with creating a better culture within academia. In my current role at the University, I combine both teaching and research activities. This gives me the unique opportunity to help to create a better and more diverse working environment. Because now that I am where I am, I have this amazing opportunity to fight for more inclusion in science, and that is a challenge I’m eager to tackle during the next decades of my career.
- King, H. W. et al. Single-cell analysis of human B cell maturation predicts how antibody class switching shapes selection dynamics. Sci Immunol. 2021; 6(56):eabe6291. doi: 10.1126/sciimmunol.abe6291
- James, L. K. and Durham, S. R. Update on mechanisms of allergen injection immunotherapy. Clin Exp Allergy. 2008; 38(7):1074-88. doi: 10.1111/j.1365-2222.2008.02976.x
- Galson, J. D. et al. Deep Sequencing of B Cell Receptor Repertoires From COVID-19 Patients Reveals Strong Convergent Immune Signatures. Front Immunol. 2020; 11:605170. doi: 10.3389/fimmu.2020.605170
- King, H. W. et al. Integrated single-cell transcriptomics and epigenomics reveals strong germinal center-associated etiology of autoimmune risk loci. bioRxiv. 2021.03.16.435578. doi: 10.1101/2021.03.16.435578