 Antibody-drug conjugates
Antibody-drug conjugates
The therapeutic potential of antibody-drug conjugates (ADCs)
To understand the therapeutic potential of antibody-drug conjugates (ADCs) it is essential to first analyze their mechanism of action, best clinical targets, and current limitations. In this article, we summarize seminal knowledge on this field and provide an overview of the most promising trends.
ADC therapy, an invaluable tool to fight cancer
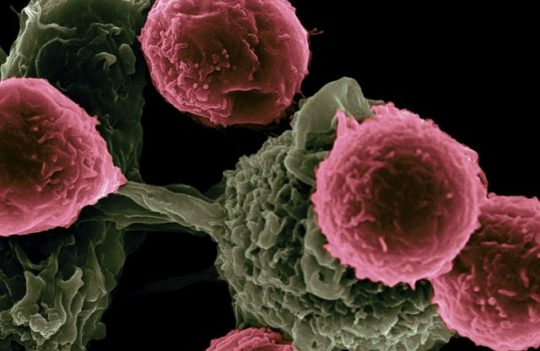
Antibody-drug conjugates (ADCs) are currently recognized as potent anti-cancer therapies targeting both solid tumors and hematological malignancies with high effectiveness. The conventional structure of ADCs consists of potent cytotoxic agents attached to an antibody carrier via a chemical linker. Dozens of ADCs have received marketing approval by the FDA in recent years and many more are currently under active clinical development.
The advantages of these therapies stem from their high target specificity allied to the potency of their toxic payloads. By acting synergistically, ADCs overcome the most common limitations of immunotherapies and chemotherapies alone – the lack of potency and excess of toxicity, respectively. With the development of new linker chemistry, conjugation technologies, and the use of new payloads, ADCs are expected to bring novel therapeutic breakthroughs in the coming decades.
Major mechanisms of action of therapeutic ADCs
ADCs can be defined as advanced delivery systems where the antibody is responsible for binding a specific surface cell receptor and the payload for exerting a biological effect. The major mechanism of action of ADCs can be described as follows:
- Biding of the antibody carrier to the specific membrane-bound receptor
- Internalization of the ADC complex by receptor-mediated endocytosis
- Maturation of the endosome and fusion with the lysosome
- Degradation of the ADC and release of the cytotoxic payload
Because this mechanism requires the efficient internalization of intact ADC molecules, linkers have been engineered for enhanced safety and targets have been selected following strict criteria. The ideal targets of ADC therapies can be summarized as follows:
- Abundantly and almost exclusively expressed in cancer cells
- Efficiently recycled by the cell
- Expected to undergo limited secretion to avoid binding ADCs in circulation, which could severely limit their therapeutic effectiveness
- Able to undergo quick and efficient internalization
- Expected to favor the appropriate trafficking route (endosomal degradation)
This has prompted the development of a robust generation of ADCs with enhanced efficiency. However, this mechanism of action has proved to be highly efficient against hematological tumors and highly limited when targeting solid tumors. In general, ADCs diffuse poorly in solid tumors due to the antigen barrier imposed by peripheral cancer cells and the large size of the ADC molecule. Next-generation ADCs have emerged with the purpose of better countering these limitations.
Currently, many ADCs have been designed to favor the use of highly efficient and specific linkers, able to release the payload in the tumor microenvironment and forgo the need for internalization. By releasing the cargo on the extracellular space, the small cytotoxic agents are free to diffuse quickly through the cell membrane and target both antigen-positive and antigen-negative cancer cells (bystander effect). This is a crucial advantage due to the heterogeneity of solid tumors and their propensity for developing resistance by mutation of surface cell receptors.
Common clinical targets of therapeutic ADCs
Dozens of ADC therapeutics have reached the clinic since the approval of Mylotarg in 2000. Currently, many more ADCs populate the clinical pipeline promising to bring new and ground-breaking tools to our anti-cancer arsenal within the next decades. Historically, ADC therapies have focused on highly abundant surface cell receptors including:
- HER2 – also known as receptor tyrosine-protein kinase erbB-2, CD340 (cluster of differentiation 340), proto-oncogene Neu, or ERBB2 protein. HER2 remains one of the most targeted receptors for the treatment of breast cancer. It is found in 30% of cancer patients and correlates with poor prognostics and with the most aggressive forms of the disease. Currently, two therapeutic ADCs in the clinic target HER2 including Kadcyla and Enhertu, both sharing the same antibody backbone but carrying different payloads.
- CD22 – it is a transmembrane glycoprotein associated with B cell malignancies such as non-Hodgkin lymphoma, and acute lymphoblastic leukemia, among others. Currently, one therapeutic ADC and one immunotoxin target this marker. The first carries a DNA-damaging agent conjugated with an anti-CD22 monoclonal antibody (Besponsa), while the second carries a fragment of Pseudomonas exotoxin A associated with an Fv fragment (Lumoxiti).
In recent years, there has been an increased interest in developing ADCs targeting solid tumors. In this context, several promising markers are currently being investigated:
- Tissue factor (TF), frequently expressed by cancer cells and is known to promote tumor growth, angiogenesis, metastasis, and thrombosis. Recently, Tivdak an anti-TF ADC was granted approval by the FDA for the treatment of cervical cancer (2021).
- Hepatocyte growth factor receptor (HGFR) or c-Met is a membrane receptor with tyrosine kinase activity. Amplification of c-Met receptors has been reported in different types of cancer, often leading to cancer cell transformation, tumor progression, and treatment resistance. Several ADCs targeting these receptors are currently in the clinical pipeline, with telisotuzumab vedotin, carrying MMAE (tubulin inhibitor), being the closest to approval.
- Folate receptor alpha (FRα), is glycosyl-phosphatidylinositol (GPI) membrane-bound glycoprotein overexpressed in several types of cancer cells with a putative role in cancer progression. Mirvetuximab soravtansine, an anti-FRα ADC carrying DM4 (tubulin inhibitor) has recently completed phase III clinical trials for the treatment of ovarian cancer with satisfactory results.
New trends in therapeutic ADC discovery
ADC therapies face three important challenges: limited efficacy against solid tumors, tumor-initiating cells (TICs), and senescent cells. Eradicating these cells while keeping systemic toxicity low is key to improving the overall prognostics of many types of cancer. With this purpose in mind, researchers are actively exploring alternative structures and strategies for therapeutic ADC development:
- Dual-targeting (bispecific antibody carrier) or dual-drug systems (two different payloads)
- Probody drug conjugates (only activated by specific enzymes)
- Engineering linkers for more efficient payload release
- Safely increase DAR (drug-to-antibody ratio) values to allow the use of less toxic payloads
- Optimize site-specific and click chemistry for conjugation to reduce the heterogeneity of ADCs
- Criscitiello, C. et al. Antibody–drug conjugates in solid tumors: a look into novel targets. J Hematol Oncol. 2021; 14(1):20. doi: 10.1186/s13045-021-01035-z
- Shim, H. Bispecific Antibodies and Antibody–Drug Conjugates for Cancer Therapy: Technological Considerations. Biomolecules. 2020; 10(3): 360. doi: 10.3390/biom10030360
- Thirlway, J. ADCs and solid tumours – The payload revolution that drives therapeutic opportunities in unmet need. Drug Discovery World. 2020; 21(2). Retrieved from: https://www.ddw-online.com/adcs-and-solid-tumours-the-payload-revolution-that-drives-therapeutic-opportunities-in-unmet-need-848-202004/
You could also be interested in: