 Peptide synthesis
Peptide synthesis
Improving vaccine development may be crucial to discern the best candidates to curb the COVID-19 pandemic
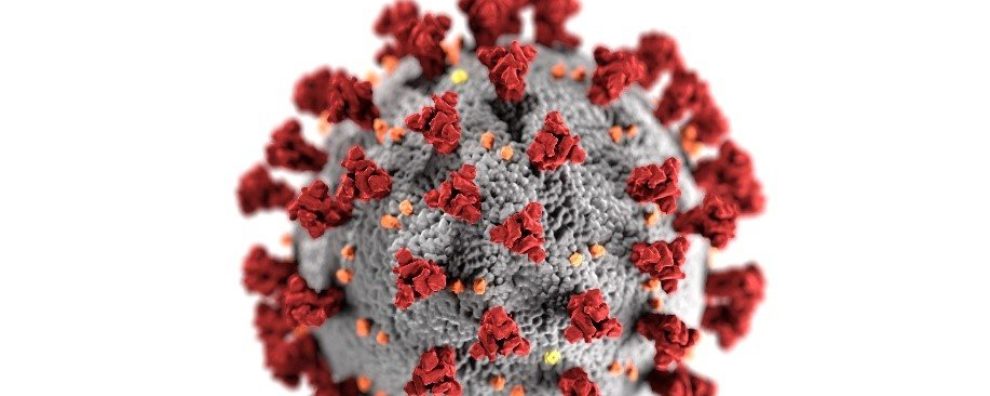
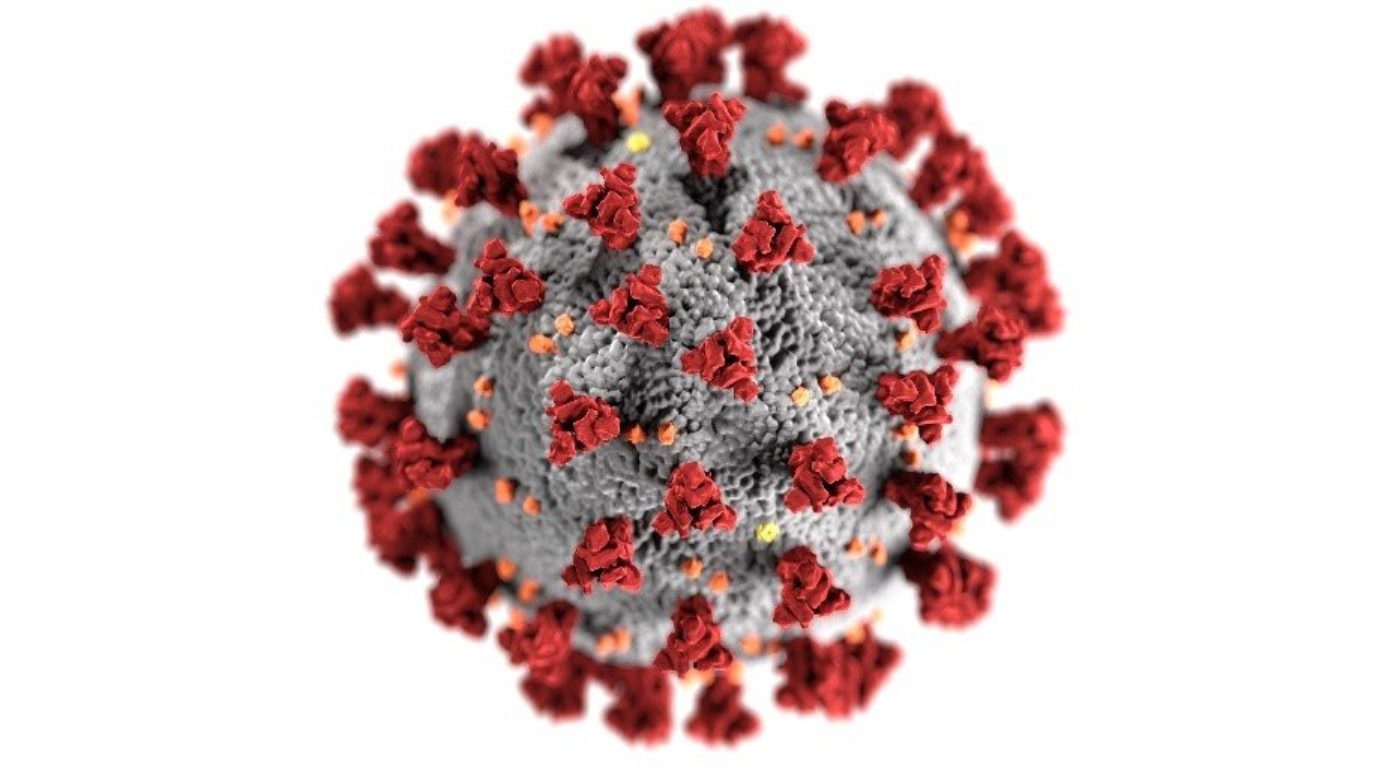
Vaccines could help us curb the COVID-19 pandemic. But vaccine efficiency can be difficult to assess during early clinical trials. The evaluation of most vaccines for COVID-19 focuses on safety and on measuring the production of protective antibodies. But an effective humoral response may be insufficient to confer long-term protection against SARS-CoV-2. For this reason, researchers are urging us to include the measurement of cell-mediated, long-term immunity during the early stages of vaccine development
COVID-19 vaccine development
Moderna has recently released early data on the clinical trial of its mRNA vaccine – mRNA-1273 – for the prophylactic treatment of COVID-19. The phase 1 trial was designed to evaluate the safety of the new vaccine, consisting of a lipid nanoparticle-encapsulated mRNA encoding for a prefusion stabilized spike glycoprotein (protein S).
Following a 2-dose vaccination schedule, the participants’ levels of anti-SARS-CoV-2 antibodies were measured by enzyme-linked immunosorbent assay (ELISA) after each dose. Two weeks following the second dose of the vaccine (day 43), the levels of anti-spike antibodies in participants’ sera were similar or higher than the levels seen in the sera of COVID-19 recovered patients.
The strength of some of the participant’s immune response was also measured by the plaque reduction neutralization test (PRNT). Unlike ELISA, which focuses solely on binding affinity to the antigen, PRNT is a sensitive, culture-dependent, and time-consuming assay designed to measure the in vitro viral neutralizing activity of sera’s antibodies.
The results of these tests, performed in 8 participants (4 from each of the cohorts, 25 and 100 µg dose levels), were consistent with the data obtained by ELISA measurements. This suggests that the mRNA vaccine was able to elicit a strong neutralizing activity against SARS-CoV-2.
Moderna’s mRNA-1273 was also found to be safe and well-tolerated among the participants of the study. Phase 3 trials are expected to begin as early as July.
But Moderna’s vaccine is only 1 of 8 candidates on clinical trials for the prophylactic treatment of COVID-19. Other candidates are based on adenovirus technologies, inactivated SARS-CoV-2 viral particles, or spike-encoding plasmid DNA.
Despite joint efforts between biotech and biopharma companies, some researchers are urging us to rethink vaccine development to improve how we assess their efficiency during early trials.
Measuring humoral and cell-mediated immunity during vaccine development
After the initial excitement over the latest COVID-19 vaccine developments, experts are raising concerns regarding the durability of the protection conferred by these new vaccines. The presence of neutralizing antibodies suggests a strong humoral response, but it fails to inform us if the vaccine was successful in activating cell-mediated immunity.
Cell-mediated immunity plays a crucial role in long-term immunologic memory. Moreover, recent studies show that T-cell activation was also observed in COVID-19 patients, suggesting these cells may be crucial for a robust immune response against the new pathogen. Studies related to other infectious diseases have also suggested there is no direct correlation between a strong humoral and strong cell-mediated response. For this reason, monitoring the immune cell population behavior during early evaluation is becoming increasingly important.
This cell-mediated immunity can be captured using flow cytometry or enzyme-linked immunoSPOT (ELISPOT) to study the subpopulation of cells in the peripheral blood, the concentration of cytokines, or chemokines, or the presence of cytotoxic activity.
In a 2018 report, the Public Health Agency of Sweden evaluated the need to include cell-mediated immunity tests in their vaccine surveillance program. In some cases, T cell immunity was found to better correlate with a protective response than high levels of antibody titers. Moreover, in the case of rubeola, evidence suggests that both humoral and cell-mediated immunity are important to control the infection.
Concluding remarks
With 8 vaccines undergoing clinical trials and dozens more under preclinical evaluation, it may be hard to differentiate the ones with better chances of eliciting a strong, effective, and long-lasting immune response.
As proposed by many experts and policymakers, the study of the cell-mediated response to a given vaccine may help us predict the outcomes of different vaccination strategies. We lack knowledge regarding the long-term behavior of SARS-CoV-2 and the complexity of the immune response it produced in our organisms. For this reason, the more vaccine development focus on capturing the complexity of our immune response, the higher the chances of discovering a truly effective vaccine.
- Moderna Announces Positive Interim Phase 1 Data for its mRNA Vaccine (mRNA-1273) Against Novel Coronavirus. May 18, 2020. Retrieved from https://investors.modernatx.com/news-releases/news-release-details/moderna-announces-positive-interim-phase-1-data-its-mrna-vaccine
- Gianchecchi, E. et al. The use of cell-mediated immunity for the evaluation of influenza vaccines: an upcoming necessity. Hum Vaccin Immunother. 2019; 15(5): 1021–1030. doi: 10.1080/21645515.2019.1565269
- Grifoni, A. et al. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020. doi: 10.1016/j.cell.2020.05.015
- Public Health Agency of Sweden. Cell mediated immunity in laboratory vaccine surveillance – a tool to better predict immunity to vaccine preventable diseases? July 24, 2018. Retrieved from https://www.folkhalsomyndigheten.se/publicerat-material/publikationsarkiv/c/cell-mediated-immunity-in-laboratory-vaccine-surveillance/
- World Health Organization (WHO). Draft landscape of COVID-19 candidate vaccines. May 15, 2020. Retrieved from https://www.who.int/who-documents-detail/draft-landscape-of-covid-19-candidate-vaccines