Antibody production
Antibody production
Fully human antibodies that will make the news in 2020
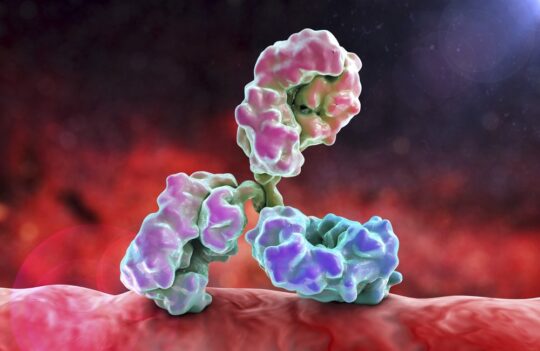
As the demand for fully human antibodies continues to rise, so does the proportion of clinical approvals of this type of biopharmaceuticals. 2020 is expected to break the all-time record of clinical approvals, and the year has already begun with the approval of Teprotumumab, a fully human antibody developed for the treatment of debilitating cases of the thyroid eye disease.
How will fully human antibodies fare in 2020?
The pipeline of antibody therapeutics is a complex one. With many of these biopharmaceuticals failing to pass preclinical and clinical trials, antibodies are still entering into the pipeline in record numbers.
The increased interest in therapeutic antibody development results in part from the high rate of success of these biomolecules (overall 22% success rate from Phase I to clinical approval). Moreover, the length of time spent in clinical development and regulatory review is widely known, varying from 4-12 years, with an average of 8 years for every new candidate.
Since 2014 an average of 8 new therapeutic antibodies have been approved in the US or the EU, every year. Although the number of approvals has been exceptionally low in 2019, with only 6 new antibodies entering the clinics, 2020 is expected to break the record of approvals.
Moreover, although Novartis’ Beovu ® (Brolucizumab) derived from the humanization of rabbit hybridoma, may have rekindled the interest in this decades-old technology, the future will likely be dominated by fully human antibodies, bispecifics, and antibody-drug conjugates.
In 2020, at least 4 fully human antibodies have been under regulatory review, 1 of them has recently gained approval in January 21 – Teprotumumab. Interestingly, Teprotumumab is also the first antibody to gain FDA approval in 2020.
Fully human antibodies to watch in 2020
Teprotumumab (Tepezza®)
Developed using Medarex’s UltiMAb® technology (transgenic mice), Teprotumumab is a fully human antibody (IgG1) targeting the insulin-like growth factor – IGF-1R. Developed by Genmab and Roche, the antibody is used for the treatment of adults suffering from thyroid eye disease.
This rare autoimmune disease where muscles and fatty tissues behind the eye become inflamed, causes the eyes to bulge outwards (proptosis). Although the disease affects only a small percentage of the adult population, its symptoms can be considered incapacitating. For instance, adults diagnosed with this condition suffer from the progressive inability to perform mundane tasks like driving, reading, sleeping and working. In some patients, the disease can even result in complete sight loss.
Until recently, these symptoms could only be alleviated through multiple invasive surgeries. Teprotumumab promises to change that by providing a simpler treatment. When administered to patients by 8 infusions every 3 weeks, the new drug led to a 2-mm or greater reduction in proptosis in comparison to the placebo group.
Narsoplimab (OMS721)
Narsoplimab is a fully human antibody (IgG4) targeting mannan-binding lectin-associated serine protease-2 (MASP-2), an important enzyme from the lectin pathway of the complement system. The drug, developed by Omeros, was designed to target and prevent complement-mediated inflammation and to not interfere with other important pathways of innate immunity.
The biopharmaceutical is currently on regulatory evaluation for the treatment of hematopoietic stem cell transplant-associated thrombotic microangiopathy (HSCT-TMA), an often-deadly and recurrent complication following stem-cell bone marrow transplants.
According to Omeros, the late-stage clinical trial data is promising, since narsoplimab considerably improved the survival of high-risk HSCT-TMA patients. If results continue to be promising, narsoplimab could become the first drug of its class able to act as a complement inhibitor and to increase the chances of survival in HSCT-TMA patients.
The condition is known to affect between 0.5-76% of patients who received a hematopoietic stem cell transplant (HSCT) and has an estimated mortality rate of 60-90%. Currently, there are no other adequate treatment options available.
REGN-EB3 and MAb114
Of the 4 fully human antibodies in review, REGN-EB3 and MAb114 are perhaps the most anticipated candidates. Both candidates were developed for the treatment of the Ebola virus disease (EVD). REGN-EB3 consists of a mixture of 3 human IgG1 (REGN3470, REGN3471, and REGN3479), while Mab114 consists of a single monoclonal antibody isolated by screening memory B cells from an Ebola survivor, 11 years after clinical infection.
Developed by immunizing transgenic mice (VelocImmune® mice, Regeneron Technology), REGN-EB3 binds to distinct nonoverlapping epitopes of Ebola’s glycoprotein, minimizing the occurrence of escape mutants. While the single human antibody – Mab114 – binds to a conserved region of the receptor-binding domain of Ebolavirus glycoprotein. This antibody remains bound to its target both in physiological pH and in intracellular pH environments, thus preventing the virus from engaging with the host’s cell receptor protein (intracellular cholesterol transporter 1 protein, NPC1) in late endosomes. The targeting of the receptor is also an ideal solution to reduce the occurrence of escape mutants, as mutations in the receptor would lead to a decrease in infection efficiency.
The Zaire ebolavirus was reported as early as 1976 and responsible for the tragic outbreak of 2013-2016 causing 11,000 deaths. The most recent outbreak of the virus, that began in 2018, has already escalated to more than 3,400 cases and resulted in more than 2,200 deaths in the Democratic Republic of the Congo and Uganda.
REGN-EB3 and MAb114 were both tested during the impressive PALM (“PAmoja TuLinde Maisha”, means together save lives in Kiswahili) clinical trial that took place in the epicenter of the Ebola outbreak. The efficiency of these two fully human antibodies was compared to that of ZMapp (a cocktail of 3 human-mouse chimeric antibodies) and remdesivir (a nucleotide analog).
The trial showed very promising results with 66.5% and 64.9% of patients who were administered REGN-EB3 and MAb114, respectively, surviving Ebola infection over 28 days. These two human-antibody-based treatments outperformed ZMapp and remdesivir, which resulted in an overall survival rate of 46.9 to 50.3%.
Concluding remarks
In 2020, the clinical approval of new therapeutic antibodies is expected to break the record of 12 FDA approved antibodies established in 2018. Interestingly, the first biopharmaceutical to gain approval in 2020 was the fully human antibody Teprotumumab, developed for the treatment of thyroid eye disease.
However, the most anticipated candidates are REGN-EB3 and MAb114, two fully human antibodies obtained through radically different approached. They both outperformed ZMapp (a chimeric human-mouse antibody cocktail) and remdesivir in the fight against life-threatening Ebolavirus infection. Their approval has the potential of mitigating the devastating effects of the ongoing Ebola outbreak that as already took the lives of more than 2,200 people since 2018.
- Choi, C. M. et al. Thrombotic microangiopathy in haematopoietic stem cell transplantation: diagnosis and treatment. Drugs. 2009;69(2):183-98. doi: 10.2165/00003495-200969020-00004
- FDA approves first treatment for thyroid eye disease. January 21, 2020. Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-thyroid-eye-disease?
- Geographical distribution of Ebola virus disease cases, DRC and Uganda. European Centre for Disease Prevention and Control. Available from: https://www.ecdc.europa.eu/en/all-topics-z/ebola-and-marburg-fevers/threats-and-outbreaks/ebola-outbreak-DRC-geographical-distribution. Last accessed on February 19, 2020
- Inserro, A. FDA Approves Biologic Teprotumumab, First Drug for Thyroid Eye Disease. AJMC. January 21, 2020. Available from: https://www.ajmc.com/newsroom/fda-approves-biologic-teprotumumab-first-drug-for-thyroid-eye-disease
- Levine, M. M. Monoclonal Antibody Therapy for Ebola Virus Disease. N Engl J Med 2019; 381:2365-2366. doi: 10.1056/NEJMe1915350