Antibody production
Antibody production
Can successful anticancer immunotherapies change the course of the COVID-19 disease?
A recent study revealed the hidden parallelisms in our organism’s response to cancer and COVID-19. Despite the marked differences between the two conditions, both seem to share a similar aberrant response in the regulation and expression of key immune checkpoint proteins. Blocking these aberrant proteins has been shown to produce durable protective effects in cancer patients. Will these inhibitory drugs be able to elicit a similar response in COVID-19 patients?
What makes us vulnerable to COVID-19?
Understanding the immune response to SARS-CoV-2 is key to propose the most effective therapeutic solutions. However, as of July 2020, there is still much we don’t know about the behavior of this new strain of coronavirus.
While most infected individuals experience only mild symptoms, a minority ends up developing severe pneumonia or, in the worst cases, acute respiratory distress syndrome (ARDS). Interestingly, these three different levels of severity have laid the groundwork for understanding what makes us vulnerable or resistant to this disease.
Moreover, determining what differs in our antiviral immune response can help us design more suitable therapeutic strategies.
In a recent study, researchers have looked into and compared the diversity and abundance of immune cells circulating in the blood of healthy individuals, COVID-19 patients with mild symptoms, pneumonia, and ARDS. The results of the study were surprising and revealed that the increased severity of symptoms was accompanied by the depletion of mature Natural Killer (NK) cells and significant changes in the expression of key immune checkpoint proteins.
These observations suggest that NK cells play a crucial role in antiviral immune responses and viral clearance and their marked depletion in patients experiencing ARDS also marks an opportunity to improve current therapeutic approaches.
Immune checkpoint inhibitors in the fight against COVID-19
Concomitant with the changes in diversity and abundance of immune cells, researchers also found increased immunosuppressive activity in the most severe cases of the COVID-19 disease. This behavior translated into an enhanced expression of surface receptors such as PD-1 (programmed cell death 1) and NKG2A (CD94/NK group 2 member A), known to possess a strong immunosuppressive effect on T and NK cells, and increased expression of CD39, known to be upregulated by hypoxia (oxygen deprivation at the tissue level).
Together, these results expose the parallelisms between our organism’s response to cancer and COVID-19. Moreover, backed by decades of cancer research, researchers can now reformulate the way we treat COVID-19 by adapting the robust anticancer strategies based on immune checkpoint inhibitors.
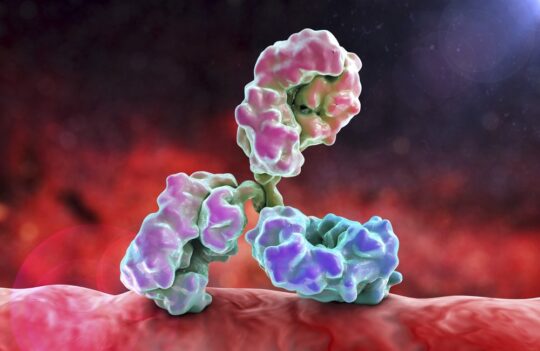
Immune checkpoints, a normal part of our immune system, are key molecules in the regulation of the intensity and specificity of the organism’s immune response. In many conditions, such as cancer, patients are known to display an aberrant checkpoint response which prevents the organism from destroying cancer cells and allows them to proliferate and metastasize.
On the contrary, in COVID-19, this aberrant response appears to be ultimately responsible for producing a broad and intense reaction that ends up destroying healthy alongside infected tissue in the upper respiratory tract leading to severe lung damage.
This aberrant behavior is regulated by immune checkpoint proteins such as PD-1, NKG2A, and CD39. Decades of research in cancer show that antibodies that block either the immune checkpoint proteins or their corresponding ligands produce durable protective responses.
Immune checkpoint inhibitors in clinical trials
Since 2011, dozens of immune checkpoint immunotherapies have been approved by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for the treatment of diverse forms of cancer. Currently, at least 4 active clinical trials are attempting to repurpose and develop PD-1 or NKG2A-blocking drugs for the treatment of COVID-19:
- Camrelizumab: a humanized IgG4 monoclonal antibody targeting the PD-1 protein, currently undergoing phase 2 clinical trials
- Nivolumab: a human IgG4 monoclonal antibody developed in transgenic mice and targeting the PD-1 protein, also undergoing phase 2 clinical trials
- Pembrolizumab: a murine humanized IgG4 monoclonal antibody targeting PD-1, currently in phase 2 clinical trials in combination with Tocilizumab (an IL-6 blocking antibody, key to reducing poor outcomes in COVID-19 patients suffering from cytokine storms)
- Monalizumab: a murine humanized IgG4 monoclonal antibody targeting the NKG2A protein, currently undergoing phase 2 clinical trials
Recent studies further showed that incubating NK cells from ARDS COVID-19 patients in vitro with Monalizumab reestablished important cellular functions. However, human clinical trials are urgently needed to understand how these drugs perform in the complex context of this disease.
Concluding remarks
Recent studies reveal that poor outcomes in COVID-19 patients may be linked to an aberrant immune response comprising the release of pro-inflammatory molecules (such as cytokines), the depletion of essential immune cells (such as NK), and upregulation of vital immune checkpoints.
Exacerbated responses have been consistently described in COVID-19 patients with severe pneumonia and ARDS. These results suggest that regulating the aberrant immune response may be vital in reducing the damage inflicted by SARS-CoV-2 on the human organism. Furthermore, the increasing parallelisms between the new viral disease and cancer have been leading researchers to repurpose common anticancer drugs for the treatment of COVID-19.
Initial studies show great promise; however, more trials and research are needed to understand the most effective dosages for the treatment of the most severe cases of the new respiratory disease.
- Demaria, O. et al. Identification of druggable inhibitory immune checkpoints on Natural Killer cells in COVID-19. Cell Mol Immunol. 2020. doi: 10.1038/s41423-020-0493-9
- Wei, S. C. et al. Fundamental Mechanisms of Immune Checkpoint Blockade Therapy. Cancer Discov. 2018; 8(9): 1069-1086. doi: 10.1158/2159-8290.CD-18-0367